Almira Mujic, Dylan Mogensen, Katelyn Bolam, Natalie Mourant
Abstract
As radiologic technologists, we are responsible for reducing patient dose while creating an image of diagnostic quality. One of the best tools to reduce patient dose, is through the use of a light beam collimator. This is attached to the x-ray tube and allows for control of the field size used when exposing the patient. We wanted to study the significance of the relationship between collimation and dose with this experiment.
Background
- X-rays are a form of energy, called radiation, that have enough energy to pass through the body
- When x-ray photons pass through the body, some of them are absorbed by the body, while the others penetrate the imaging plate behind the patient to create an image
- Tissues that are thicker and have a higher atomic number are more sensitive to radiation and have a higher radiation dose
- Thicker tissue requires a higher technique (or more x-rays) to create a diagnostic image
Collimation Standards
Currently, there are no institutional or national standards regarding collimation in the field of radiography.
Radiographic textbooks recommend collimating on all four sides of the anatomy of interest or to 1 cm of light beyond the edge of anatomy.
These are only recommendations for radiographers as there are no requirements.
How does an x-ray compare to your natural exposure to radiation?
| Exam | Dose mSv | Equivalent time in natural background radiation |
|---|---|---|
| Chest x-ray | 0.1 | 10 days |
| L-Spine x-ray | 1.5 mSv | 6 months |
| Hand x-ray | 0.001 mSv | 3 hours |
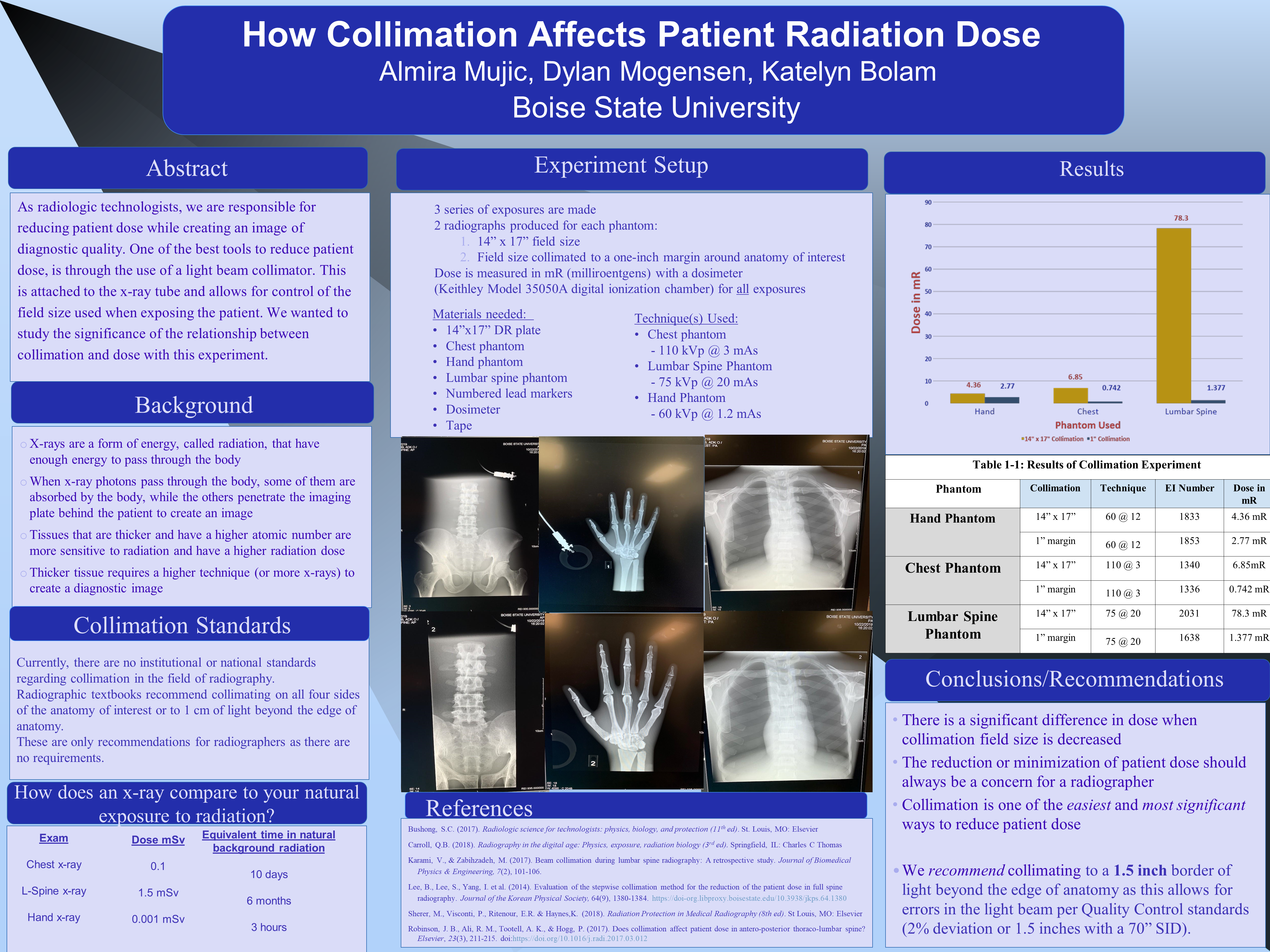
Experiment Setup
3 series of exposures are made
2 radiographs produced for each phantom:
- 14” x 17” field size
- Field size collimated to a one-inch margin around anatomy of interest
Dose is measured in mR (milliroentgens) with a dosimeter
(Keithley Model 35050A digital ionization chamber) for all exposures
Materials needed:
- 14”x17” DR plate
- Chest phantom
- Hand phantom
- Lumbar spine phantom
- Numbered lead markers
- Dosimeter
- Tape
Technique(s) Used:
- Chest phantom, 110 kVp @ 3 mAs
- Lumbar Spine Phantom, 75 kVp @ 20 mAs
- Hand Phantom, 60 kVp @ 1.2 mAs
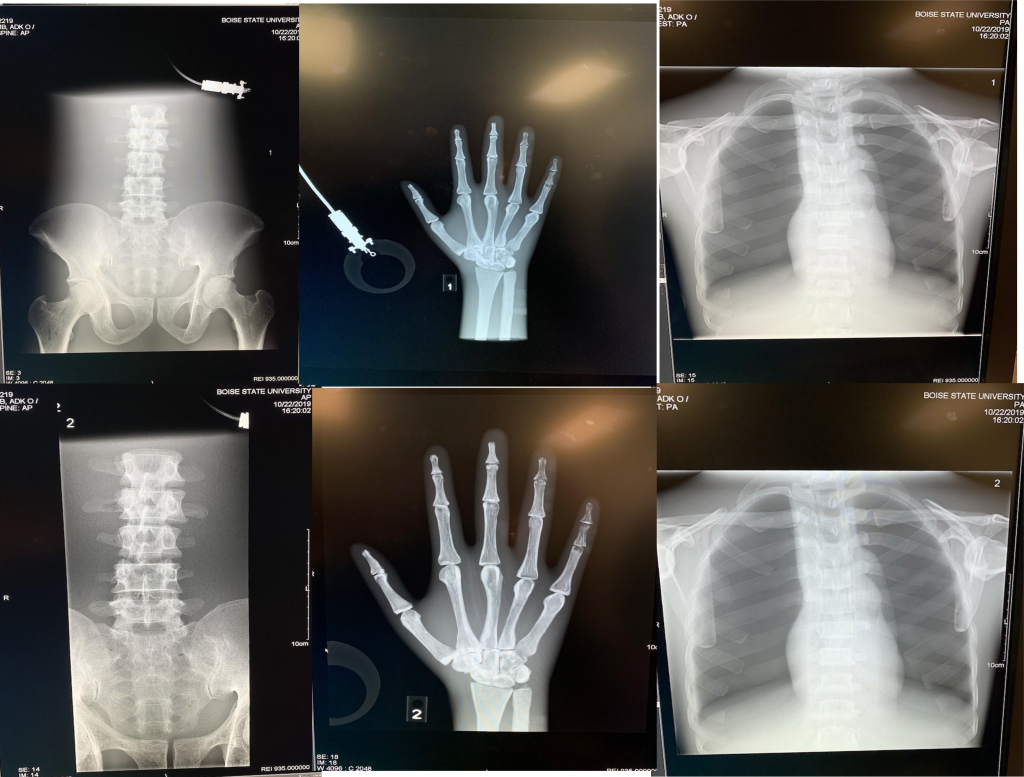
Results
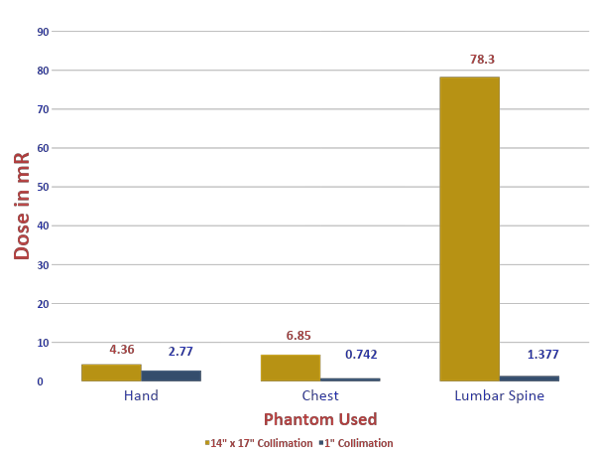
Table 1-1: Results of Collimation Experiment
| Phantom | Collimation | Technique | EI Number | Dose in mR |
|---|---|---|---|---|
| Hand | 14” x 17” | 60 @ 12 | 1833 | 4.36 mR |
| Hand | 1” margin | 60 @ 12 | 1853 | 2.77 mR |
| Chest | 14” x 17” | 110 @ 3 | 1340 | 6.85mR |
| Chest | 1” margin | 110 @ 3 | 1336 | 0.742 mR |
| Lumbar Spine | 14” x 17” | 75 @ 20 | 2031 | 78.3 mR |
| Lumbar Spine | 1” margin | 75 @ 20 | 1638 | 1.377 mR |
Conclusions/Recommendations
- There is a significant difference in dose when collimation field size is decreased
- The reduction or minimization of patient dose should always be a concern for a radiographer
- Collimation is one of the easiest and most significant ways to reduce patient dose
- We recommend collimating to a 1.5 inch border of light beyond the edge of anatomy as this allows for errors in the light beam per Quality Control standards (2% deviation or 1.5 inches with a 70” SID).
References
- Bushong, S.C. (2017). Radiologic science for technologists: physics, biology, and protection (11th ed). St. Louis, MO: Elsevier
- Carroll, Q.B. (2018). Radiography in the digital age: Physics, exposure, radiation biology (3rd ed). Springfield, IL: Charles C Thomas
- Karami, V., & Zabihzadeh, M. (2017). Beam collimation during lumbar spine radiography: A retrospective study. Journal of Biomedical Physics & Engineering, 7(2), 101-106.
- Lee, B., Lee, S., Yang, I. et al. (2014). Evaluation of the stepwise collimation method for the reduction of the patient dose in full spine radiography. Journal of the Korean Physical Society, 64(9), 1380-1384. https://doi-org.libproxy.boisestate.edu/10.3938/jkps.64.1380
- Sherer, M., Visconti, P., Ritenour, E.R. & Haynes,K. (2018). Radiation Protection in Medical Radiography (8th ed). St Louis, MO: Elsevier
- Robinson, J. B., Ali, R. M., Tootell, A. K., & Hogg, P. (2017). Does collimation affect patient dose in antero-posterior thoraco-lumbar spine? Elsevier, 23(3), 211-215. doi:https://doi.org/10.1016/j.radi.2017.03.012
Additional Information
For questions or comments about this research, contact Dylan Mogensen at dylanmogensen@u.boisestate.edu.