Megan Anne West, Camille Hinchcliff, Morgan Sorg, Lonny Ashworth
Background
Airway Pressure Release Ventilation (APRV) is a form of pressure controlled intermittent mandatory ventilation that is designed to allow unrestricted spontaneous breathing through the breath cycle, especially during Timehigh (Thigh). APRV is applied using I:E ratios much greater than 1:1 or inverse ratio ventilation, usually relying on short expiratory times and gas trapping (AutoPEEP) to maintain end-expiratory lung volume, rather than with a preset PEEP. APRV may improve oxygenation and decrease the amount of alveolar derecruitment during the Timelow (Tlow). The purpose of this bench study was to evaluate APRV and its ability to create AutoPEEP on the Carefusion Avea (Avea) in APRV/BiLevel, Drager V500 (V500) in PC-APRV, Medtronics Puritan Bennett 980 (PB 980) in BiLevel, and Maquet Servo-i (Servo-i) in BiVent when connected to the IngMar Medical ASL 5000 (ASL) electronic lung simulator with a passive lung model set at three levels of static compliance to simulate three severities of ARDS.
Methods
An extended self-test was performed on each ventilator using oxygen and air. ASL settings for severity of ARDS: Compliance (CST) 40 ml/cm H2O (mild ARDS), 30 ml/cm H2O (moderate ARDS), and 20 ml/cm H2O (severe ARDS); inspiratory resistance 12 cm H2O/L/s, expiratory resistance 14 cm H2O/L/s, and Pmus 0 cm H2O (passive lung model).
The ASL was connected directly to the ventilator Y-piece with a 22 mm adapter. Ventilator settings: pressure high (Phigh) set at 17 cm H2O for the first trial and 22 cm H2O for the subsequent trial, Thigh 6 seconds , pressure low ( Plow) at 0 cm H2O, Tlow was adjusted to achieve a release point at 75% of peak expiratory flow rate (PEFR), according to the Habashi Method; pressure support (PS) 0 cm H2O, and tube compensation off. PEFR was measured directly from the ventilator flow vs. time waveforms.
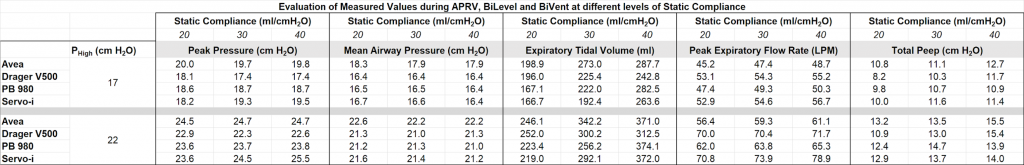
Each trial consisted of ventilating the ASL lung model for one minute to stabilize values and one minute for data collection. Each ventilator was tested with a Phigh 17 cm H2O (2 minutes total), then at Phigh of 22 cm H2O (2 minutes total) testing the highest CST 40 ml/cm H2O first. The trial was repeated at CST 30 ml/cm H2O, and finally at CST 20 ml/cm H2O. Data were recorded directly by the ASL and the parameters evaluated include: PEFR, peak inspiratory pressure (PIP), mean airway pressure (MAP), total PEEP (PEEPtot), and expiratory tidal volume (VTE).
Results
Phigh 22 cm H2O resulted in an increase of all evaluated parameters compared to Phigh 17 cm H2O. The change in CST had a strong direct linear correlation to the change in VTE. The Avea had the highest PIP, highest MAP, and lowest PEFR at each level of compliance and both levels of Phigh, and had the highest PEEPtot in most cases. In severe ARDS, the Avea and the V500 exhibited the greatest VTE at both levels of Phigh and the V500 had the lowest PEEPtot at both levels of Phigh. See the Table.
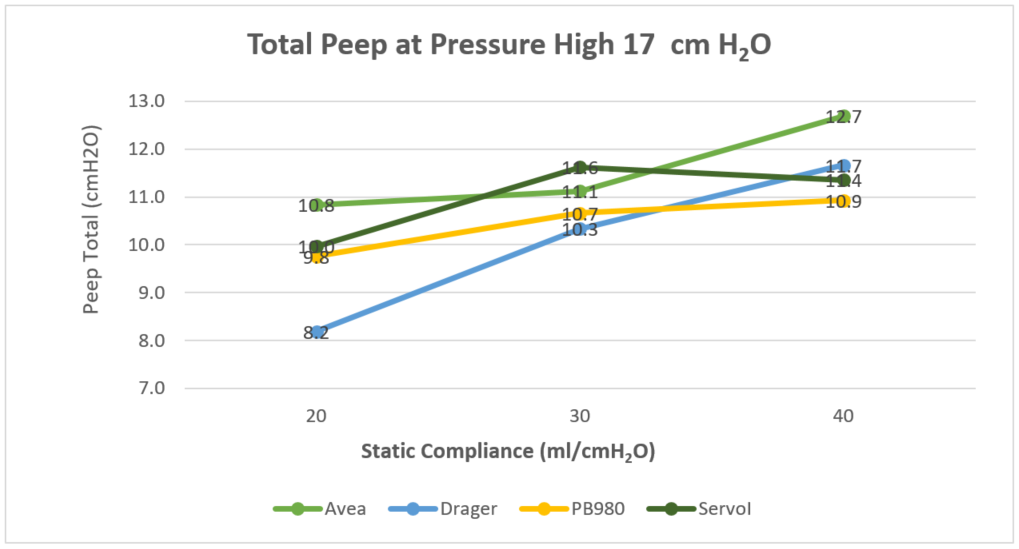
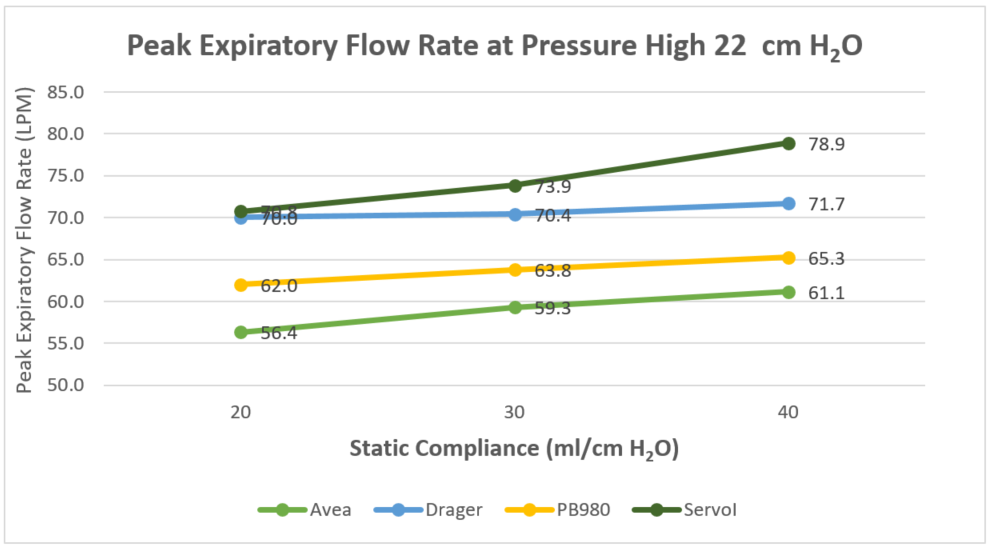
Table 1: Evaluation of Measured Values during APRV, BiLevel and BiVent at different levels of Static Compliance
Conclusion
This study demonstrated that all ventilators provided an increase in PEEPTOTt, VTE , MAP, PEFR, and PIP at Phigh 22 cm H2O when compared to Phigh 17 cm H2O. Each ventilator, compared to the others, provided a different level of PEFR and PEEPtot at 75% PEFR, even when they were set to the same Phigh; this is probably due to the difference in the resistance among the ventilators caused by the exhalation valve. Further research is needed to compare APRV in patients with different severities of ARDS to determine the amount of gas trapping that occurs by measuring PEEPtot at 75% PEFR in order to prevent derecruitment of lung. Additional clinical studies on patients are needed to evaluate the differences and effectiveness of APRV used on different ventilators.
Limitations
Some ventilators did not allow for a Tlow short enough to have expiration end and inspiration begin at 75% PEFR. Due to this limitation it is important to take into consideration that some ventilators may have resulted in a PEFR less than 75% PEFR leading to the potential for an increase in VTE, a decrease in PEEPtot and an increase in lung derecruitment at the end of Tlow. This limitation resulted in some of the ventilators unable to fully meet the parameters of the Habashi Method.
References
Arnal JM, Garnero A, Saoli M, Chatburn RL. Parameters for Simulation of Adult Subjects During Mechanical Ventilation. Respir Care 2018;63(2):158-168.
No authors have a conflict of interest related to this research. No authors have received research funding, sponsorship or financial support from companies related to this research.
Additional Information

For questions or comments about this research, contact Megan Anne West at meganwest@u.boisestate.edu.