Shaylynn Giroir, Lauren Mattaini, Diana Stelmakh, Kendal Sweet, Natalie Mourant
Abstract
The purpose of this research is to review and represent the data collected on breast tissue dose as it relates to full spine radiography to grasp a better understanding of how patient positioning affects the dose to breast tissue. Utilizing radiographic phantoms and a dosimeter, radiation measurements were noted in conjunction with the positioning techniques used by practicing technologists. The primary goal of the research is to educate radiographers on breast tissue dose in different scoliosis positioning in order to make decisions that benefit the patient and follow the rules of ALARA (as low as reasonably achievable).
Objectives
- To determine the ideal position for patients receiving full spine radiography while saving dose to breast tissue.
- Null 1: There is no significant difference in dose to breast tissue when positioning patients in anteroposterior (AP) versus posteroanterior (PA) for a scoliosis series when holding all other variables constant.
- Null 2: There is no significant difference in dose to breast tissue when utilizing a compensating filter for a scoliosis series.
Materials
- Quantum Imaging X-ray System with Carestream Retrofit
- 14 x 17 inch direct conversion receptor plate
- Thorax Phantom
- Fluke Triad Biomedical dosimeter
- Ferlic compensating filter
- Silk tape
- Lead marker
Methods
- Position the thorax phantom upright in front of the wall bucky in an AP position.
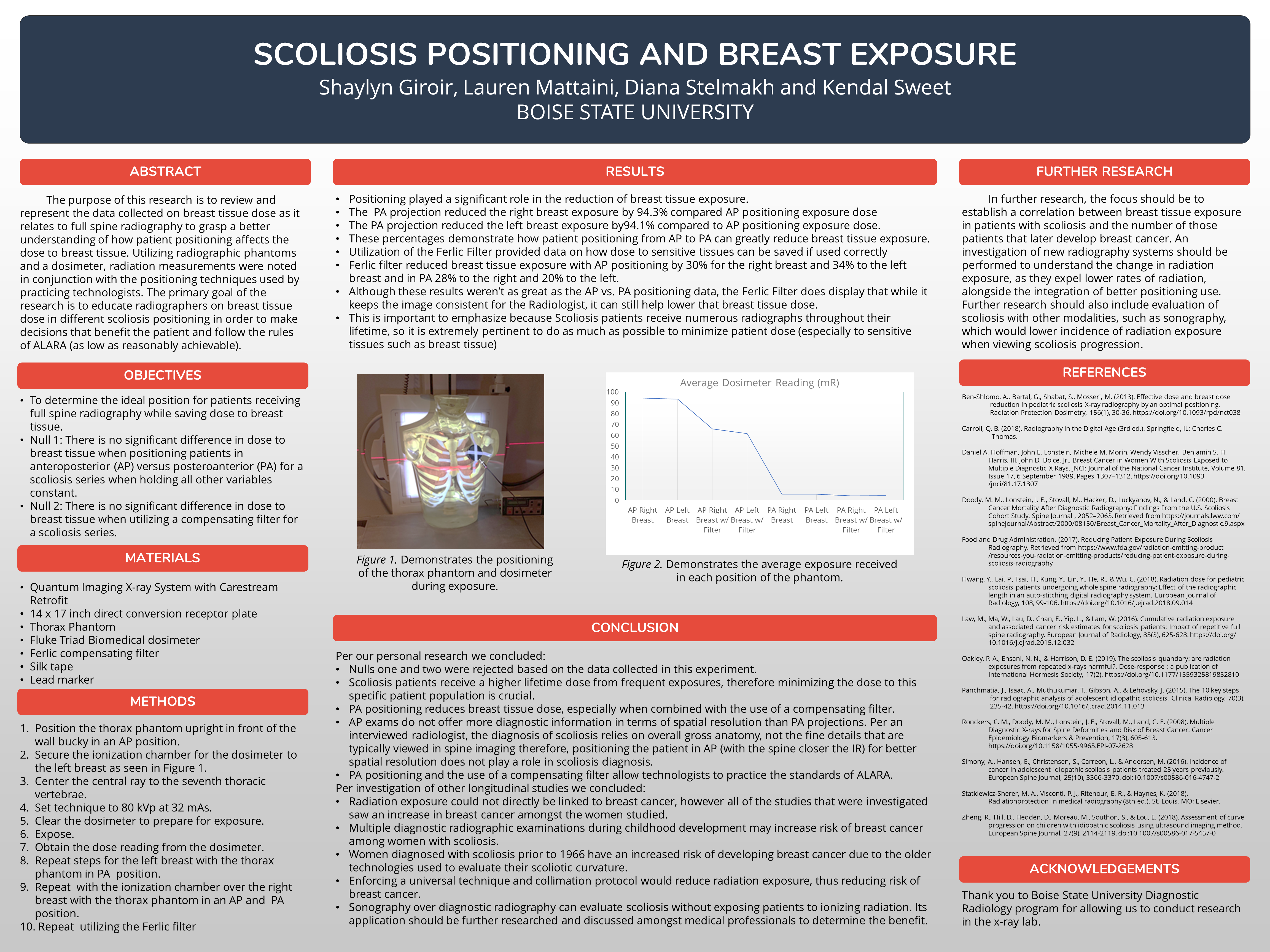
- Secure the ionization chamber for the dosimeter to the left breast as seen in Figure 1.
- Center the central ray to the seventh thoracic vertebrae.
- Set technique to 80 kVp at 32 mAs.
- Clear the dosimeter to prepare for exposure.
- Expose.
- Obtain the dose reading from the dosimeter.
- Repeat steps for the left breast with the thorax phantom in PA position.
- Repeat with the ionization chamber over the right breast with the thorax phantom in an AP and PA position.
- Repeat utilizing the Ferlic filter
Results
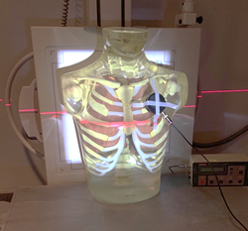
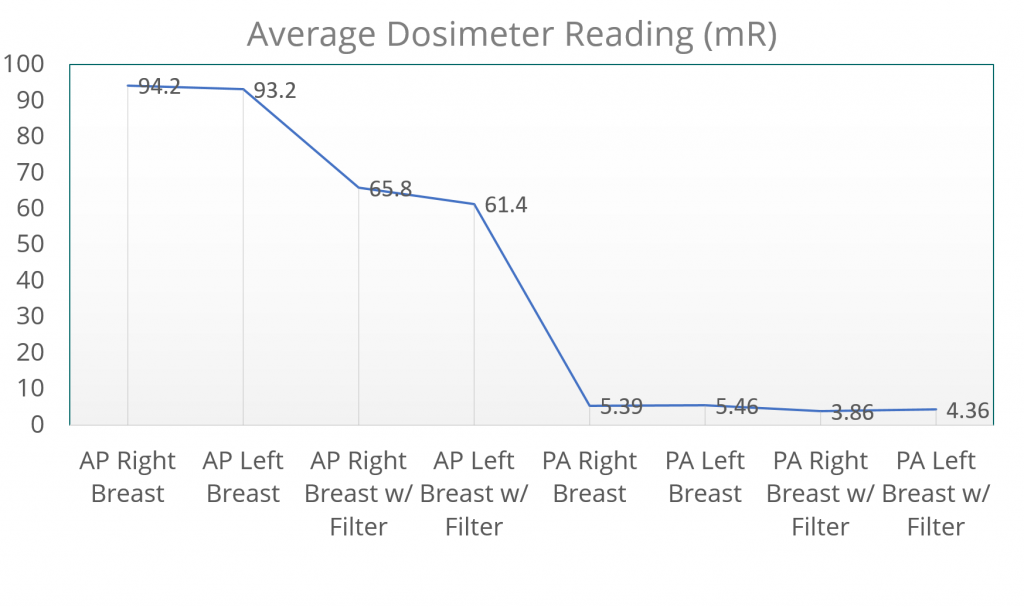
- Positioning played a significant role in the reduction of breast tissue exposure.
- The PA projection reduced the right breast exposure by 94.3% compared AP positioning exposure dose
- The PA projection reduced the left breast exposure by 94.1% compared to AP positioning exposure dose.
- These percentages demonstrate how patient positioning from AP to PA can greatly reduce breast tissue exposure.
- Utilization of the Ferlic Filter provided data on how dose to sensitive tissues can be saved if used correctly
- Ferlic filter reduced breast tissue exposure with AP positioning by 30% for the right breast and 34% to the left breast and in PA 28% to the right and 20% to the left.
- Although these results weren’t as great as the AP vs. PA positioning data, the Ferlic Filter does display that while it keeps the image consistent for the Radiologist, it can still help lower that breast tissue dose.
- This is important to emphasize because Scoliosis patients receive numerous radiographs throughout their lifetime, so it is extremely pertinent to do as much as possible to minimize patient dose (especially to sensitive tissues such as breast tissue)
Conclusion
Per our personal research we concluded:
Nulls one and two were rejected based on the data collected in this experiment.
Scoliosis patients receive a higher lifetime dose from frequent exposures, therefore minimizing the dose to this specific patient population is crucial.
PA positioning reduces breast tissue dose, especially when combined with the use of a compensating filter.
AP exams do not offer more diagnostic information in terms of spatial resolution than PA projections. Per an interviewed radiologist, the diagnosis of scoliosis relies on overall gross anatomy, not the fine details that are typically viewed in spine imaging therefore, positioning the patient in AP (with the spine closer the IR) for better spatial resolution does not play a role in scoliosis diagnosis.
PA positioning and the use of a compensating filter allow technologists to practice the standards of ALARA.
Per investigation of other longitudinal studies we concluded:
- Radiation exposure could not directly be linked to breast cancer, however all of the studies that were investigated saw an increase in breast cancer amongst the women studied.
- Multiple diagnostic radiographic examinations during childhood development may increase risk of breast cancer among women with scoliosis.
- Women diagnosed with scoliosis prior to 1966 have an increased risk of developing breast cancer due to the older technologies used to evaluate their scoliotic curvature.
- Enforcing a universal technique and collimation protocol would reduce radiation exposure, thus reducing risk of breast cancer.
- Sonography over diagnostic radiography can evaluate scoliosis without exposing patients to ionizing radiation. Its application should be further researched and discussed amongst medical professionals to determine the benefit.
Further Research
In further research, the focus should be to establish a correlation between breast tissue exposure in patients with scoliosis and the number of those patients that later develop breast cancer. An investigation of new radiography systems should be performed to understand the change in radiation exposure, as they expel lower rates of radiation, alongside the integration of better positioning use. Further research should also include evaluation of scoliosis with other modalities, such as sonography, which would lower incidence of radiation exposure when viewing scoliosis progression.
References
- Ben-Shlomo, A., Bartal, G., Shabat, S., Mosseri, M. (2013). Effective dose and breast dose reduction in pediatric scoliosis X-ray radiography by an optimal positioning, Radiation Protection Dosimetry, 156(1), 30-36. https://doi.org/10.1093/rpd/nct038
- Carroll, Q. B. (2018). Radiography in the Digital Age (3rd ed.). Springfield, IL: Charles C. Thomas.
- Daniel A. Hoffman, John E. Lonstein, Michele M. Morin, Wendy Visscher, Benjamin S. H. Harris, III, John D. Boice, Jr., Breast Cancer in Women With Scoliosis Exposed to Multiple Diagnostic X Rays, JNCI: Journal of the National Cancer Institute, Volume 81, Issue 17, 6 September 1989, Pages 1307–1312, https://doi.org/10.1093 /jnci/81.17.1307
- Doody, M. M., Lonstein, J. E., Stovall, M., Hacker, D., Luckyanov, N., & Land, C. (2000). Breast Cancer Mortality After Diagnostic Radiography: Findings From the U.S. Scoliosis Cohort Study. Spine Journal , 2052–2063. Retrieved from https://journals.lww.com/ spinejournal/Abstract/2000/08150/Breast_Cancer_Mortality_After_Diagnostic.9.aspx
- Food and Drug Administration. (2017). Reducing Patient Exposure During Scoliosis Radiography. Retrieved from https://www.fda.gov/radiation-emitting-product
/resources-you-radiation-emitting-products/reducing-patient-exposure-during-
scoliosis-radiography - Hwang, Y., Lai, P., Tsai, H., Kung, Y., Lin, Y., He, R., & Wu, C. (2018). Radiation dose for pediatric scoliosis patients undergoing whole spine radiography: Effect of the radiographic length in an auto-stitching digital radiography system. European Journal of Radiology, 108, 99-106. https://doi.org/10.1016/j.ejrad.2018.09.014
- Law, M., Ma, W., Lau, D., Chan, E., Yip, L., & Lam, W. (2016). Cumulative radiation exposure and associated cancer risk estimates for scoliosis patients: Impact of repetitive full spine radiography. European Journal of Radiology, 85(3), 625-628. https://doi.org/ 10.1016/j.ejrad.2015.12.032
- Oakley, P. A., Ehsani, N. N., & Harrison, D. E. (2019). The scoliosis quandary: are radiation exposures from repeated x-rays harmful?. Dose-response : a publication of International Hormesis Society, 17(2). https://doi.org/10.1177/1559325819852810
- Panchmatia, J., Isaac, A., Muthukumar, T., Gibson, A., & Lehovsky, J. (2015). The 10 key steps for radiographic analysis of adolescent idiopathic scoliosis. Clinical Radiology, 70(3), 235-42. https://doi.org/10.1016/j.crad.2014.11.013
- Ronckers, C. M., Doody, M. M., Lonstein, J. E., Stovall, M., Land, C. E. (2008). Multiple Diagnostic X-rays for Spine Deformities and Risk of Breast Cancer. Cancer Epidemiology Biomarkers & Prevention, 17(3), 605-613. https://doi.org/10.1158/1055-9965.EPI-07-2628
- Simony, A., Hansen, E., Christensen, S., Carreon, L., & Andersen, M. (2016). Incidence of cancer in adolescent idiopathic scoliosis patients treated 25 years previously. European Spine Journal, 25(10), 3366-3370. doi:10.1007/s00586-016-4747-2
- Statkiewicz-Sherer, M. A., Visconti, P. J., Ritenour, E. R., & Haynes, K. (2018). Radiationprotection in medical radiography (8th ed.). St. Louis, MO: Elsevier.
- Zheng, R., Hill, D., Hedden, D., Moreau, M., Southon, S., & Lou, E. (2018). Assessment of curve progression on children with idiopathic scoliosis using ultrasound imaging method. European Spine Journal, 27(9), 2114-2119. doi:10.1007/s00586-017-5457-0
Acknowledgements
Thank you to Boise State University Diagnostic Radiology program for allowing us to conduct research in the x-ray lab.
Additional Information
For questions or comments about this research, contact Shaylynn Giroir at shaylynngiroir@u.boisestate.edu.