Aline Bates, Chelsea Clower, Madison Koster, Madison Wirth, Michael Johnson, Natalie Mourant
Radiologic Sciences, Department of Health Sciences
Background

“Shielding” in radiography is the process of utilizing lead drapes and coverings of different shapes and sizes for the purpose of reducing patient exposure by radiation. This reduction in patient dose is achieved by absorption of x-rays by lead shielding rather than by the body. Gonadal shielding is a type of shielding designed and shaped specifically for the more highly sensitive male and female gonadal tissues.
The practice of gonadal shielding within the radiologic community has long been under debate. However,beginning in2019, the American Association of Physicists in Medicine (AAPM) released a statement endorsing the discontinuation of gonadal shielding due to technological advancement and research demonstrating negligible radiation risk for non-shielded vs. shielded patients1. The American College of Radiology has supported this statement, however, many radiologic organizations call for more research.
Members and facilities associated with the American Society of Radiologic Technologists (ASRT) have voiced concerns over the shift in policyand in response have recommend more research is necessary to determine the efficiencyof shieldingbefore endorsing the new AAPM stance on shielding.2
The purpose of this study was to collect radiation exposure data specific to the use of gonadal shielding and determine if shielding should continue as a best practice in patient radiation exposure reduction.
Methodology
A test was conducted to determine the efficacy of gonadal shielding in reducing dose for patients and whether the long-standing practice of shielding is warranted. Three phantoms were used for this experiment: a pelvis, a foot, and a chest. For all experiments, the pelvis phantom had a dosimeter placed in the estimated area the ovaries would lie in a female patient. They were conducted using a 0.5 mm lead equivalent shield for three exposures, and then again without the shielding for three exposures. The averages were calculated for each condition.


Should We Shield Our Patients?

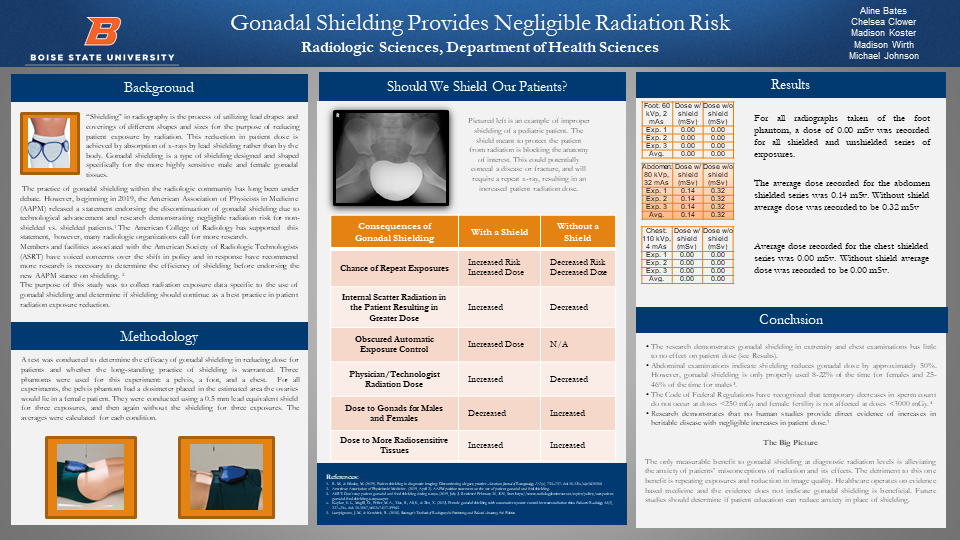
Pictured left is an example of improper shielding of a pediatric patient. The shield meant to protect the patient from radiation is blocking the anatomy of interest. This could potentially conceal a disease or fracture, and will require a repeat x-ray, resulting in an increased patient radiation dose.
| Consequences of Gonadal Shielding | With a Shield | Without a Shield |
|---|---|---|
| Chances of Repeat Exposures | Increased Risk, Increased Dose | Decreased Risk, Decreased Dose |
| Internal Scatter Radiation in the Patient Resulting in Greater Dose | Increase | Decreased |
| Obscured Automatic Exposure Control | Increased Dose | N/A |
| Physician/Technologist | Increased | Decreased |
| Dose to Gonads for Males and Females | Decreased | Increased |
| Dose to More Radiosensitive Tissues | Increase | Decreased |
Results
For all radiographs taken of the foot phantom, a dose of 0.00 mSv was recorded for all shielded and unshielded series of exposures.
| Foot: 60 kVp, 2mAs | Dose w/shield (mSv) | Dose w/o shield (mSv) |
|---|---|---|
| Exp 1 | 0.00 | 0.00 |
| Exp 2 | 0.00 | 0.00 |
| Exp 3 | 0.00 | 0.00 |
| Avg | 0.00 | 0.00 |
The average dose recorded for the abdomen shielded series was 0.14 mSv. Without shield average dose was recorded to be 0.32 mSv
| Abdomen: 80 kVp, 32 mAs | Dose w/shield (mSv) | Dose w/o shield (mSv) |
|---|---|---|
| Exp 1 | 0.14 | 0.32 |
| Exp 2 | 0.14 | 0.32 |
| Exp 3 | 0.14 | 0.32 |
| Avg | 0.14 | 0.32 |
Average dose recorded for the chest shielded series was 0.00 mSv. Without shield average dose was recorded to be 0.00 mSv.
| Chest: 110 kVp, 4 mAs | Dose w/shield (mSv) | Dose w/o shield (mSv) |
|---|---|---|
| Exp 1 | 0.00 | 0.00 |
| Exp 2 | 0.00 | 0.00 |
| Exp 3 | 0.00 | 0.00 |
| Avg | 0.00 | 0.00 |
Conclusion
- The research demonstrates gonadal shielding in extremity and chest examinations has little to no effect on patient dose (see Results).
- Abdominal examinations indicate shielding reduces gonadal dose by approximately 50%. However, gonadal shielding is only properly used 8-22% of the time for females and 25-46% of the time for males3.
- The Code of Federal Regulations have recognized that temporary decreases in sperm count do not occur at doses <250 mGyand female fertility is not affected at doses <3000 mGy.4
- Research demonstrates that no human studies provide direct evidence of increases in heritable disease with negligible increases in patient dose.1
The Big Picture
The only measurable benefit to gonadal shielding at diagnostic radiation levels is alleviating the anxiety of patients’ misconceptions of radiation and its effects. The detriment to this one benefit is repeating exposures and reduction in image quality. Healthcare operates on evidence based medicine and the evidence does not indicate gonadal shielding is beneficial. Future studies should determine if patient education can reduce anxiety in place of shielding.
References
- R. M., & Silosky, M. (2019). Patient shielding in diagnostic imaging: Discontinuing a legacy practice. American Journal of Roentgenology, 212(4), 755–757. doi: 10.2214/ajr.18.20508
- American Association of Physicists in Medicine. (2019, April 2). AAPM position statement on the use of patient gonadal and fetal shielding.
- ASRT: Don’t stop patient gonadal and fetal shielding during x-rays. (2019, July 2). Retrieved February 20, 2020, from https://www.radiologybusiness.com/topics/policy/asrt-patient-gonadal-fetal-shielding-x-rays-aapm
- Kaplan, S. L., Magill, D., Felice, M. A., Xiao, R., Ali, S., & Zhu, X. (2012). Female gonadal shielding with automatic exposure control increases radiation risks. Pediatric Radiology, 48(2), 227–234. doi: 10.1007/s00247-017-3996-5
- Lampignano, J. M., & Kendrick, R. (2018). Bontrager’s Textbook of Radiographic Positioning and Related Anatomy, 9th Edition
Additional Information
For questions or comments about this research, contact Aline Bates at alinebates@u.boisestate.edu.