Concussions have dominated contact sports conversations in recent years – most notably in the National Football League, where players have been diagnosed with the degenerative brain disease Chronic Traumatic Encephalopathy (CTE), associated with repetitive brain trauma.

However, few studies have examined the impacts concussions have on the youngest participants in youth sports. Boise State University researchers teamed up with a cohort of professionals from St. Luke’s Applied Research Division in 2016 to measure changes in the flow of fluid across white matter tracts in the brain before and after a youth football season.
“The more we looked into the literature, we realized there was a lack of information about changes in youth that may occur over a season,” explained Leslie Kendrick, an associate professor and program director for radiologic sciences at Boise State. “That’s why we chose young male football players.”
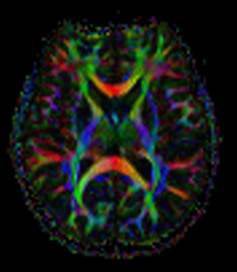
White matter is specific tissue within the brain and spinal cord that acts as a path of communication, akin to an electrical wire between the two, and helps guide our motor control, among other things. When white matter pathways are healthy and undisturbed, water in the brain generally flows across them in a single direction. When there is damage and swelling, this can be assessed as the water in the brain starts to diffuse more randomly, and this injury interferes with the relay of information to and from the brain.
“One of the major concerns with concussion is that it can cause a disruption in the flow of fluid across white matter tracks,” Kendrick explained.
Kendrick was joined by Yong Gao, a professor of kinesiology; Hilary Flint, St. Luke’s applied research manager; and Dr. Kurt Nilsson, the medical director of the St. Luke’s Sports Medicine Concussion Clinic. Flint, along with the research coordinators from the St. Luke’s Applied Research Division, conducted the recruitment and coordination of 35 youth football players, ages 8-12, to undergo magnetic resonance imaging (MRI) scans of their brains before their football season and again immediately following the season. As a control group, the researchers also imaged the white matter fluid pathways via MRI of 12 male swimmers of the same age.
The football players were outfitted with accelerometers from Shockbox® throughout the football season – technology that recorded the number, magnitude and direction of impacts – in their helmets. The devices pair with smartphones, which allowed the tracking the g-force of hits in real- time on the field.
“The sensors tallied the number, direction and g-force of each hit received during practice and games,” said Kendrick.
Steve Cutchin, an associate professor of computer science, worked with three Boise State students to select, test and calibrate the accelerometers. The sensors were set to register hits above 30 Gs. In general, a 50-60 g-force is on par with two helmets colliding, Kendrick explained.
A total of 1,905 hits were recorded during the football season. At the end of eight weeks, Gao conducted the data analysis to compare the pre and post-season MRI DTI data of both swimmers and football players, along with the accelerometer hit data of football players to gauge whether there were any statistically significant differences. The short answer as to whether significant differences were found? No.
“Overall, there were no statistically significant structural differences,” Kendrick said. “However, the data did demonstrate a pattern. As the total magnitude of hits per player increased, there was a greater difference in diffusion of fluid across the white matter in the region of the left cingulate cortex of the brain from pre- to post season.
Dr. Nilsson noted that the clinical implications of this finding still are unknown.
“In short, it’s too soon to tell,” he said. “The results suggest that there does not appear to be a significant group change in white matter structure in youth football players from pre- to post-season, nor does there seem to be a group difference between youth football players and youth swimmers, but there is a correlation between total magnitude of head impacts over a season and accumulation of white matter fluid content over a season of youth football.”
“The data did not demonstrate that children should not play football. The data did demonstrate a pattern that should be considered,” Kendrick added, “which leaves the door open for additional research.”
Kendrick and Dr. Nilsson both recognized that the study could not have happened without community partnerships.
“This is research that couldn’t have been done in any other way – this project required an intersection of the outreach relationships St. Luke’s has in the community with Boise Optimist Youth Football, the clinical expertise of St. Luke’s Sports Medicine Concussion Clinic and Boise Radiology Group, the research expertise from St. Luke’s Applied Research, and the expertise in biostatistics, computer science and radiological sciences from Boise State,” Nilsson said.
The team is working to develop a new study with youth athletes that will measure proteins released in the blood following a sports related concussion in comparison to early exercise intervention and post-concussive symptom recovery, defined as a return to work, play and learn.