Pesticide Exposure and Risk Perceptions among Men and Women Latinx Farmworkers in Idaho
This summary report provides details about the researchers key takeaways, methods, results, conclusions, and recommendations.
Download Printable Report: Pesticide Exposure and Risk Perceptions (PDF)
Key Takeaways
- Many different pesticides were found in urine samples collected from Latinx farmworkers in Idaho
- Barriers to wearing Personal Protective Equipment (PPE) include heat and believing it is not important, particularly among men
- Farmworkers said they were worried about pesticide drift and lack of notification when pesticides are sprayed on nearby farms
- Farmworkers want more interactive and in-person safety trainings
- Current regulations may not address farmworkers’ concerns, even at farms that meet all legal requirements
Authors
Carly Hyland, PhD, MS
School of Public Health, UC Berkeley / UC Agriculture and Natural Resources / School of Public and Population Health, Boise State University.
chyland@berkeley.edu
Lisa Meierotto, PhD, MA
School of Public Service, Boise State University.
lisameierotto@boisestate.edu
Rebecca Som Castellano, PhD, MA
School of the Environment / Department of Sociology, Boise State University. rsomcastellano@boisestate.edu
Cynthia Curl, PhD, MS
School of Public and Population Health, Boise State University. cynthiacurl@boisestate.edu
Irene Ruiz, MA
Idaho Organization of Resource Councils.
iruiz@iorcifo.org
Executive Summary
Latinx farmworkers represent over 80% of the agricultural workforce in the United States. Previous studies have shown that farmworkers have high levels of exposure to pesticides. However, most of those studies have focused on men. Women are becoming more visible in agriculture and it is important to understand how pesticides affect women farmworkers. We conducted a study from April-July 2022 with Latinx farmworkers in Southwestern Idaho. In this study, we measured pesticide levels in urine samples collected from farmworkers. Every participant’s urine tested positive for at least one pesticide. The farmworkers in this study expressed concerns about not being notified about pesticide spraying, particularly on nearby farms. They also wanted more hands-on and in- person pesticide safety training.
Introduction
The majority of the agricultural workforce in the US is Latinx (83%). There have been numerous studies that have shown high levels of pesticide exposure in farmworkers. However, most of these studies have focused on men (1-8) and it is important to understand pesticide exposure and the experiences of women farmworkers. Women are increasing in the agricultural workforce in the United States and globally. (9) Further, women may have a higher rate of Acute Pesticide Poisoning (APPs) compared with men farmworkers. (10-12) An APP is illness within 48 hours of exposure to a pesticide, and can cause a range of effects such as headaches, nausea, vomiting, and dizziness. It is also critical (13) to understand how farmworkers think about pesticides and their ability to protect themselves, including whether men and women protect themselves differently.
We conducted a study from April-July, 2022 with Latinx farmworkers in Southwestern Idaho. We collected urine samples to measure exposure to several agricultural pesticides. We also used questionnaires and interviews to understand a number of factors, such as what participants thought about the risks and benefits of pesticides, what behaviors they used to reduce pesticide exposure, and whether participants felt they had control to avoid pesticides.
What is the WPS?
The Worker Protection Standards (WPS) is a regulation issued by the Environmental Protection Agency (EPA). This is the main legislation in the U.S. that aims to reduce the harmful effects of pesticides. WPS training is required for agricultural workers and pesticide handlers. The primary goals are to educate workers about:
- How to prevent pesticide exposure during and after work
- How to recognize and understand signs notifying workers to keep out of pesticide-treated fields
- Sources of pesticide exposure during work (e.g., pesticide residues on crops or from pesticide drift)
- Ways to minimize pesticide exposure (e.g., wearing PPE and washing hands with soap and water while working, especially before eating or drinking)
- How to recognize the signs and symptoms of acute pesticide poisoning and when to seek medical attention
What is an agricultural worker vs. a pesticide handler?
According to the EPA, an agricultural worker is someone who “performs tasks related to the growing and harvesting of plants on farms or in greenhouses, nurseries, or forests”. A pesticide handler is someone who (14):
- Mixes, loads, or applies pesticides
- Cleans or repairs pesticide application equipment
- Helps with the application of pesticides
What are the requirements under the WPS?
The WPS explains that agricultural employers must meet certain requirements to protect workers from pesticides, relating to: 1) training and 2) notification of pesticide applications. (15) Employers of all agricultural workers are required to:
- Make sure that workers receive pesticide safety training at least once a year
- Notify workers on the establishment if they will come within a quarter mile of an area that is being treated with pesticides or that is under a Restricted Entry Interval (REI). The workers must be told verbally or there must be a written warning sign in the field.
- There must be an “ample” supply of water, soap, and towels
Additionally, employers of pesticide handlers are required to: (14, 16)
- Ensure workers receive pesticide handler safety training at least once a year
- Provide handlers with information about the pesticides they are using, including safety information about each pesticide
- If the handler is not able to understand the pesticide label, the employer is required to have someone available to explain safety information and directions for use
- Provide a respirator and fit-testing, training, and a medical evaluation, for pesticides that require a respirator
- Provide, clean, maintain, store, and ensure the use of all required PPE
- Provide decontamination supplies
RESEARCH AIMS
There were two main goals of this study:
Goal 1
Measure levels of pesticides in samples of farmworkers’ urine.
Goal 2
Understand farmworkers’ thoughts about the risks and benefits of pesticides, the amount of control they feel they have to protect themselves from pesticides, and the steps they take to protect themselves.
METHODS
Our study team included faculty and students from Boise State University and a farmworker advocate from the Idaho Organization of Resource Councils (IORC). We conducted the study from April 24, 2022, to July 22, 2022. We asked participants to complete questionnaires and interviews, and also collected urine samples from farmworkers to test for pesticides.
Participants were from the Southwestern region of Idaho and lived or worked in Nampa, Caldwell, Marsing, Mountain Home, Emmett, Homedale, Parma, Payette, and Ontario, Oregon. We recruited participants by working with local health districts, housing authorities, mobile health clinics, and events such as farmworker appreciation events. Our bilingual (English/Spanish) staff would talk with potential participants, explain the study, and see if they were eligible to participate.
The participants had to be:
- 18 years or older
- Identify as Latino/Latina or Hispanic
- Currently work in crop production
- Speak Spanish or English
Participants were also asked to self-identify as a man, woman, or other/non-binary.
If the individual was willing and able to participate in the study, a staff member read the informed consent to explain the goals and the procedures of the study. We read the informed consent in English or Spanish, depending on what the participants preferred. We then arranged a time and location that was convenient for the participant to meet to do the study. We took various measures to prioritize the participants’ security and privacy. All research activities were reviewed and approved by the Boise State University Institutional Review Board.
Pesticide Exposure Assessment
We had two study visits with each participant, within a seven-day period. During each visit, the participant answered a questionnaire and gave a urine sample. After the second visit, we combined the two urine samples to estimate their exposure over one full week. We tested for levels of herbicides, pyrethroid insecticides, and organophosphate (OP) insecticides, or their breakdown products.
Questionnaires
Participants completed a questionnaire at the two different study visits. The first questionnaire was longer and included questions about their demographic information, work history, what types of crops they worked with, and PPE use. We also asked about pesticide protective behaviors (PPBs), which are behaviors farmworkers can take to reduce their pesticide exposure. For example, we asked questions such as how often they wash their hands with soap and water during work. We also asked participants about how much control they believe they have to reduce harmful impacts of pesticides and who they believe is responsible for protecting farmworkers from pesticides.
Participants completed a short follow-up questionnaire at the second study visit. This focused on whether pesticides had been applied at the field where they work, and whether they used PPE while working in the last three days.
Semi-Structured Interviews
Eighteen (18) participants completed a longer interview. This included 11 women and 7 men. These interviews allowed participants to talk in more detail about their experiences with and beliefs about pesticides. For example, we asked their thoughts about the risks and benefits of pesticides and their experiences working in agriculture. The interviews were around 45-60 minutes long.
Demographic Characteristics
We enrolled a total of 62 farmworkers. There were 30 who self-identified as men and 32 who self-identified as women.
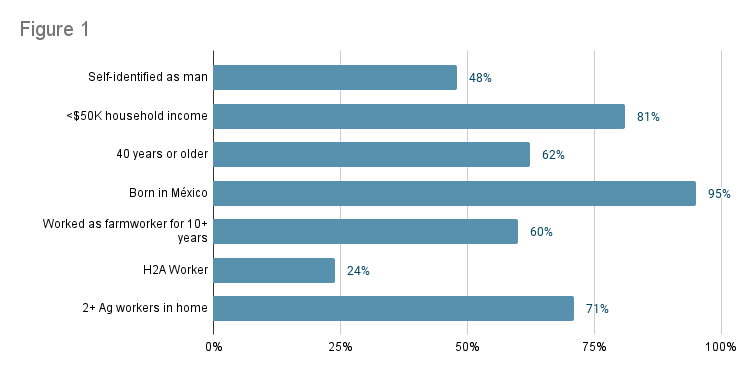
Figure 1 shows some characteristics of the study population. Of the 30 men, 15 were workers on the H2A visa program (24.1% of overall study population). The majority of the participants self-identified as Mexican (88.7%). Permanent residents had lived in the U.S. for an average of 22.5 years. H2A visa holders had been coming to the U.S. to work seasonally for an average of 9.8 years. The average age of the participants was 45.1 years old. Most participants (80.6%) had an annual household income of less than $50,000. Participants lived in homes with an average of 4.6 people, including about 2.6 other agricultural workers.
48%
81%
62%
95%
60%
24%
71%
Pesticide Concentrations
All participants provided at least one urine sample. There were 57 (92%) participants that provided two urine samples. We analyzed 17 pesticides or breakdown products that indicate exposure to pesticides. We call these pesticides and breakdown products “biomarkers”. Of these 17 biomarkers, some are not very commonly used, and these results focus on the main 11 that we thought were most important. The herbicides biomarkers we tested were 2,4-D, Glyphosate (G), Dicamba, and AMPA. We tested biomarkers of pyrethroid insecticides including 3-PBA, 4-F-3-PBA, cis-DCCA, and trans-DCCA. Biomarkers of OP insecticides included TCPy, MDA, and PNP. Most (69-100%) of participants’ samples tested positive for these biomarkers. All 62 participants had at least one of these main biomarkers detected in their samples, and 33 (53.2%) had all of these biomarkers detected in their urine.
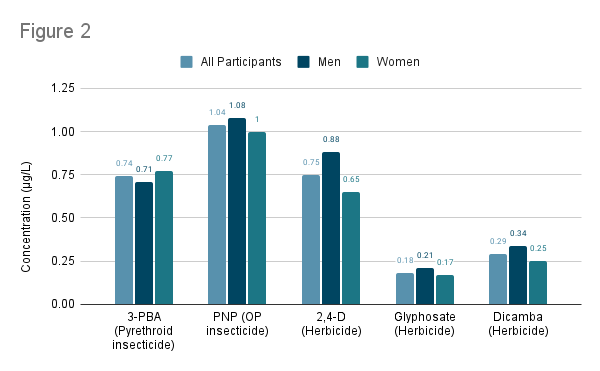
Figure 2 shows the concentrations (Geometric Mean (GM)) of some of the pesticide biomarkers that we measured in participants’ urine samples. The results are shown among all participants and separated by gender. Overall, we observed very similar pesticide biomarker concentrations among men and women.
3-PBA
PNP
2,4-D
G
Dicamba
Occupational Characteristics – Type of Crop
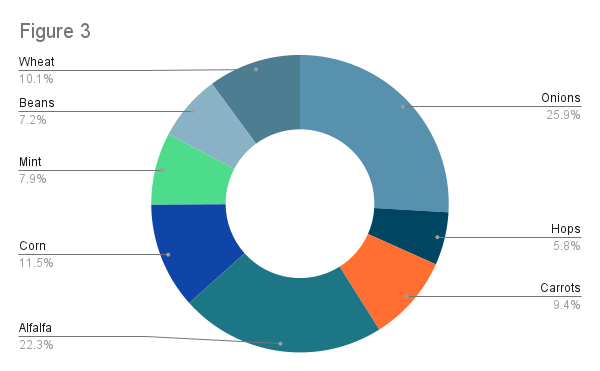
Figure 3 shows each of the crops that participants worked with within the three days prior to either study visit (participants could select multiple options). The most common crops were onions (58.1% of participants), alfalfa (50.0% of participants), and corn (25.8% of participants).
10.1%
7.2%
7.9%
11.5%
22.3%
25.9%
5.8%
9.4%
Occupational Characteristics – Types of Duties
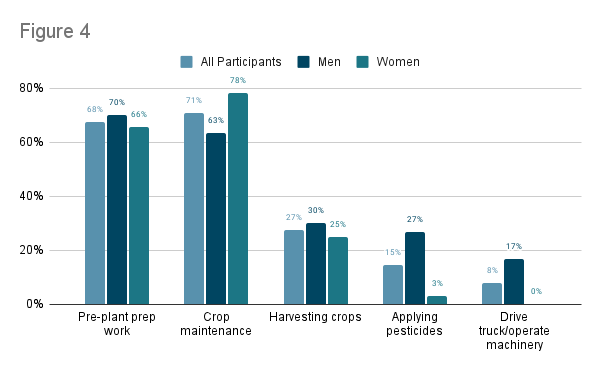
As noted by Figure 4, participants reported completing various different agricultural duties. Men and women generally performed similar tasks at work, with some exceptions. Men were significantly more likely to have mixed, loaded, or applied pesticides compared with women (26.7% of men vs. 3.1% of women). Men were also more likely to drive a truck or operate machinery (16.7% of men vs. 0% of women).
Women reported working fewer hours per week compared to men (mean = 53.9 hours/week for men and 45.1 hours/week for women). A similar percentage of men (73.3%) and women (71.9%) reported having received pesticide safety training.
Women were more likely to self-report an Acute Pesticide Poisoning (APP) (n=8, 25.9% for women; n=4, 13.8% for men).
Prep
Maint.
Harvest
Pest. Ap
Mach. Op
Pesticide Protective Behaviors
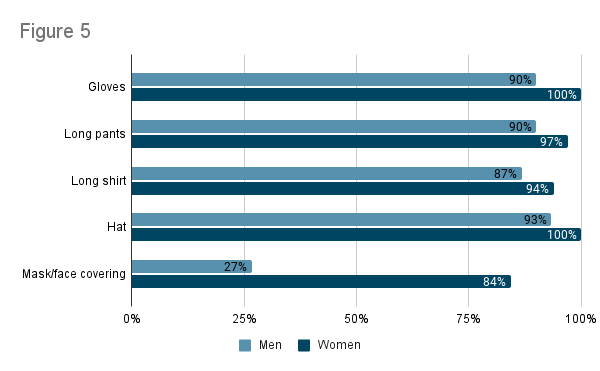
Women were slightly more likely to wear most types of PPE (Figure 5). For example, a greater proportion of women reported typically wearing gloves, long pants, a long shirt, and a hat while working in the fields. A much larger percentage of women reported wearing a mask/face covering compared with men (84.4% of women compared with 26.7% of men).
On the survey we asked participants why they didn’t wear PPE more frequently while working in the fields. The most frequent responses were that it is too hot outside (40.3% of all participants), that PPE is uncomfortable (38.7% of all participants), and that PPE is not important (16.1% of all participants).
These findings from the questionnaire are supported by participants’ comments from the open-ended interviews. For instance, nine women from the interviews mentioned they think men take more risks with pesticides than women.
Gloves
Pants
Shirt
Hat
Mask
What Participants Are Saying
“Yes, I think that men are less careful than women…we protect ourselves with hats and all that. And men don’t give it as much importance. I think maybe…they don’t think it will harm them. I’ve seen men working without gloves and other types of protection.”Participant Comment
Pesticide Applicators
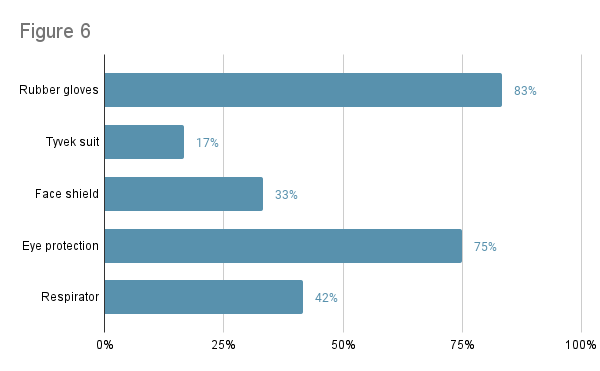
We also asked questions specific to pesticide applicators, defined as those who had mixed, loaded, or applied pesticides in the last year (10 men, 2 women).
We found that 8 participants (66.7%) had ever attended pesticide handler safety training. Of these 8 participants, 4 (33.3%) reported having received the training in the last year, as required by WPS.
Most participants who applied pesticides typically wore rubber gloves (83%) and eye protection (75%) while applying pesticides (Figure 6). Less than half wore a respirator (42%), face shield (33%), or Tyvek suit (17%) while applying pesticides (Figure 6). None of the pesticide applicators reported having their respirator fit tested, as required by WPS.
The most common reasons pesticide applicators didn’t wear PPE more often were that PPE is uncomfortable (50.0% of participants), that it is too hot outside (58.3%), and that they forget to wear PPE or don’t have access (33.3% each).
83%
17%
33%
75%
42%
Perceived Pesticide Risk
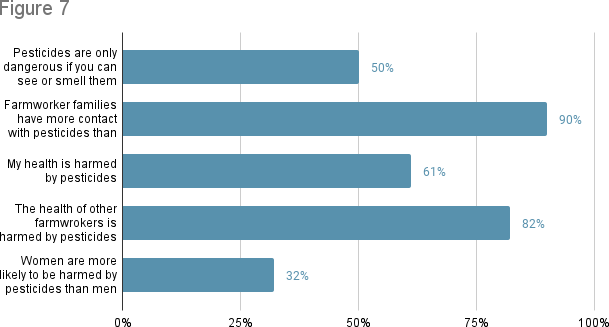
We asked participants whether they agreed with various statements about the risks of pesticides. The percentage of participants who agreed with each of these statements is shown in Figure 7. Overall, the responses between men and women were very similar. Over half of the participants agreed that pesticides are harmful to their overall health (61%). Even more (82%) agreed that pesticides affect the health of other farmworkers.
50%
90%
61%
82%
32%
Perceived Control
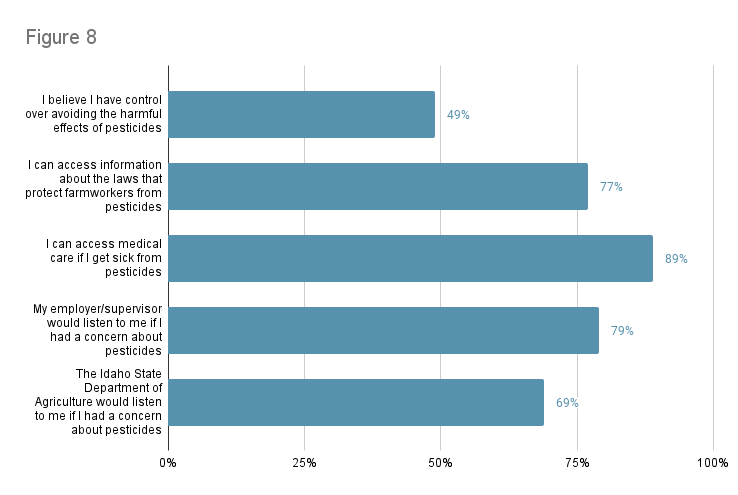
We asked participants about whether they agreed with statements about their control to avoid pesticide exposure or the harmful effects of pesticides (Figure 8). Less than half (49%) agreed with the statement that they have control to avoid the harmful effects of pesticides. Most believed they could access medical care if they got sick from pesticides (89%) and felt they had information about the laws that protect farmworkers from pesticides (77%). Over three-quarters agreed that their employer/supervisor would listen to them if they were concerned about pesticides (79%). Fewer farmworkers agreed that the Idaho State Department of Agriculture (ISDA) would listen to them if they were concerned about pesticides (69%).
49%
77%
89%
79%
69%
Indicators of Compliance with WPS
“I remember we were harvesting and a little plane passed by very close by fumigating another field next to us. So, I don’t know if it’s something that won’t hurt us or if they don’t care. I don’t know. And they say that when they put chemicals on a field, they put a sign up or something like that. When they put that sign up, they don’t have us go in there, but the sprayers, the tractors pass close by and that doesn’t – that’s what happens, they don’t let us know that much. They don’t care that much about letting us know.”Participant Comment
Forty-five participants (72.6%) reported having attended pesticide safety training, which is required by the WPS for all agricultural workers. However, the quality of this training was a concern to some of the participants. Many participants reported receiving the training from a video. While this method of training meets legal requirements, participants said these videos were not engaging or effective. Participants wanted in-person training, which would be more engaging and allow them to ask questions.
Participants also voiced concerns, particularly in the interviews, about not knowing when pesticides are sprayed at the field where they work, particularly in the open-ended interviews. When participants were notified about pesticide applications, the most common way they were notified was being told by a supervisor (80.7%), and signs being posted in the field in English (64.5%), Spanish (50.0%), or both English and Spanish (45.2%). Participants were also concerned about pesticides drifting from nearby farms to where they are working.
“They could communicate a bit more between themselves and communicate with us as workers…the workers of the other farmer should let the others know and say, ‘Hey your people are there, so get out.’ Because sometimes you get there and you smell it… sometimes you’re in the field, but the neighbor is spraying. They aren’t spraying in your work site, but someone else is spraying and it makes it to you.”Participant Comment
“There were four or five of us who were coming out of the wheat, and you can’t see us. The wheat is high…the plane went by and I just saw the downfall, and I could feel the chemicals fell on me.”Participant Comment
“And then one year…when we were working on the beets… and we were in the fields and we saw the plane go by like that and he just passed and sprayed over us and we dropped in the field, and I had my little boy, he was three years old, and he saw it and he fell on the row of the beets and he was crawling and everyone got sprayed on the back with white stuff on them. We all got sprayed. But I guess – at that time, nobody reported anything. So, we just changed our clothes and keep on going.”Participant Comment
Handwashing
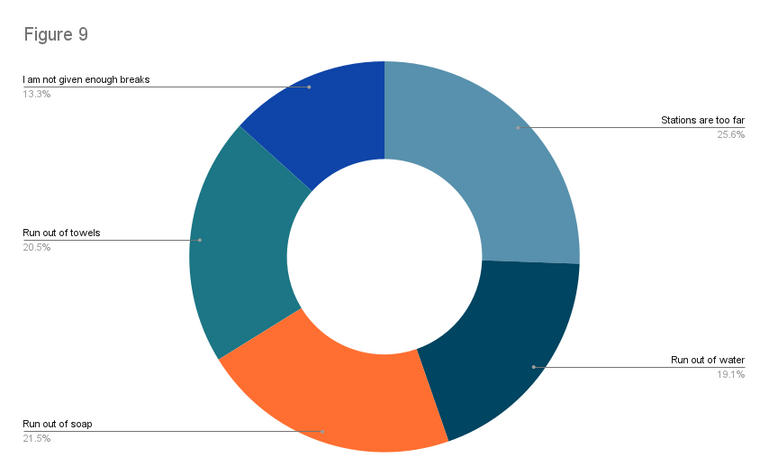
Participants told us they had various obstacles to washing their hands at work (Figure 9). The most common obstacles were the hand washing stations being too far from where they work (40.3% of participants), the hand washing stations running out of soap (33.9%), water (30.1%), or towels (32.3%). Seven participants (11.3%) indicated that they do not have hand washing stations available where they are working. Participants also said that the hand washing stations are very dirty and that there are not enough hand washing stations for the number of employees. One participant noted there is “pressure to only use [the hand washing stations] if necessary to deter laziness”.
“They don’t bring you any water. You are the one who has to bring your water to wash your hands or your hand sanitizer.”Participant Comment
Participants reported solutions such as using the bathroom in the fields or bringing their own water and/or hand sanitizer to work to wash their hands. Notably, hand sanitizer is not a WPS-endorsed way to remove pesticide residues.
“The bathroom is nearby, but sometimes there’s no water. Sometimes I have water with me, but I also forget to bring it. I have a case of bottled water inside my car. Just in case I need it.”Participant Comment
13.3%
20.5%
21.5%
25.6%
19.1%
Other Findings
Perceived Risk of Herbicides
While herbicides are not inherently less dangerous than other pesticides, participants reported they felt them to be less dangerous. They also said they were told that they don’t need the same safety precautions when using herbicides. One participant reported that they do not have a pesticide applicator license and they do not consider themselves to be a pesticide applicator because they only spray herbicides. Some of the participants reported that they do not wear PPE while working with herbicides. These findings may contribute to the higher levels of herbicides we found among pesticide applicators compared with non-applicators. These beliefs also conflict with WPS, which indicates that farmworkers should follow the guidelines on each specific pesticide product. The WPS does not indicate that herbicides are inherently safer.
Unique Experiences of Women
We found that women worked fewer hours than men and were more likely to wear most types of PPE, but more women reported having experienced an acute pesticide poisoning (APP). While there is a need for more studies, we have some potential hypotheses for this trend. First, the wide range of different jobs by gender could impact exposure to pesticides. For example, men in our study were more likely to drive trucks or operate heavy machinery. These activities may have a lower potential for pesticide exposure compared to tasks that were more common among women, such as weeding and thinning crops. Second, multiple women described that they had been poisoned from aerial pesticide spraying. It is possible that women are more likely to work with crops that are sprayed aerially. This might increase the risk for APP if proper precautions are not followed. Third, women may be more susceptible to pesticides than men due to their biological makeup. Finally, there may be differences in access to pesticide safety training. It is also possible that women do not have proper access to PPE that fits them. A combination of these factors may impact women’s exposure to pesticides and should be examined in larger studies.
Climate Change and Heat
“What worries me most is that we are going to be poisoned from pesticides…we don’t wear masks because of the temperatures and the sun.”Participant Comment
We found that farmworkers are concerned about climate change-related hazards. Participants were particularly concerned about working in extreme heat. They expressed that they are unable to work in extreme heat and have no options to protect themselves because they needed to get paid. Some said they did not use PPE because of the heat. This is concerning because PPE is one of the ways farmworkers can protect themselves from pesticides. Participants also felt that more pesticides were used in the 2022 agricultural season due to abnormally cool temperatures and increased precipitation that delayed planting.
“To gain time, since it’s a bit slow, they put more chemicals…There have been years where the weather is good, and you can plant well…and they don’t apply pesticides as often. I don’t know how much they apply, but they are applying more [pesticides].”Participant Comment
Some participants worked in both Oregon and Idaho and reported that they got more breaks while working in hot weather in Oregon. For example, one participant said “The only thing that I know is that the laws in Oregon are a bit more strict. What I understand is that in Oregon, they give you two 10 or 15 minute breaks by law, plus lunch. I think that here in Idaho, the break isn’t required, beside lunch. And in Oregon – I think after 100 degrees, you can’t work.”
“The sun does affect us…when it’s about noon, you don’t want to be there anymore because the sun is getting higher and the temperature is increasing and you can’t take it. But you have to be there working your hours because of your needs.”Participant Comment
CONCLUSION
We found frequent detections of common agricultural pesticides in urine samples collected from Latinx farmworkers in Idaho. Participants generally had similar concentrations compared to farmworkers in other studies. There was no obvious difference in pesticide concentrations between men and women, but there were some differences in questionnaire and interview responses. Women worked fewer hours than men, were less likely to be a pesticide applicator, and reported slightly higher use of PPE. In theory, these factors should reduce women’s exposure to pesticides. However, we found no difference in pesticide levels between men and women, and women were more likely to report APPs than men. This is in line with other research, and differences in pesticide exposure and the experiences of farmworkers by gender should be examined in a larger study.
Participants faced some barriers to protecting themselves from pesticides. Participants had unpredictable access to hand washing stations and bathrooms with soap, water, and towels. They also reported inconsistent notification when pesticides were used at or near the field where they work. Those handling pesticides were rarely given information about which pesticides they were using, which is necessary to follow the proper safety precautions.
Our results showed that there is a vital need for the enforcement of regulations. The information shared by farmworkers in the open-ended interviews also suggested that the current regulations, even if appropriately enforced, may not adequately protect farmworkers. One of the biggest concerns of participants in our study is the potential for pesticides to drift from nearby farms to where they are working. Current regulations do not require notification of pesticide use on adjacent farms. It is also important to note that a lot of the changes needed to protect farmworkers from pesticides are often outside of the control of farmworkers. We advocate for increased protection, such as employers provisioning of PPE, ensuring farmworkers understand what pesticides they are in contact with and the necessary safety precautions, and more engaging and in-person pesticide safety training.
RECOMMENDATIONS
Based on our findings we have developed the following specific recommendations to increase farmworkers’ protection from pesticides:
1. Improved pesticide safety training, especially in-person training.
- Videos appear to be one of the most common methods of providing pesticide safety training and, while compliant with existing regulations, may not be very effective.
- We encourage implementation of more engaging trainings, such as in-person trainings and “train-the-trainer” sessions.
- Trainings should allow participants to ask questions and interact with other farmworkers and the instructor.
2. Enhanced communication regarding pesticide products that farmworker sare handling, including all relevant safety requirements.
- Pesticide handlers are expected to read and understand complex pesticide safety labels. Handlers are also expected to follow the proper safety precautions and wear the required personal protective equipment PPE.
- Farmworkers reported they are not always informed of the products they use and may not be able to follow the appropriate safety precautions. Many pesticide handlers are not provided with the required PPE.
- The formatting of pesticide safety labels is hard to read. Safety labels are printed in English, while most farmworkers speak Spanish or another language.
- Farmworkers should be provided with clear information about what pesticides they are using and should be provided with the appropriate PPE.
3. Improved communication about pesticide applications on and near fields where people are working
- Farmworkers are often not notified about pesticide applications at the field where they work. When they are notified, there is inconsistency in how they are told (for example, verbal notification vs. warning sign). Signs are often posted far away from where they are working.
- This has resulted in farmworkers reporting confusion about when/where pesticides are being sprayed and some being poisoned.
- The current regulations do not address participants concerns. The WPS only requires notification of pesticide use within a specific zone, which is typically 25 or 100 feet. Participants reported being exposed to pesticides outside of that zone and wanting information about when pesticides are applied on other farms.
- Many of the participants expressed that increased communication between farm owners and farmworkers is necessary, including between farms.
4. Improved regulations and enforcement regarding hand washing stations and bathrooms at the workplace
- WPS encourages washing hands while working to reduce pesticide exposure. It is also important to wash hands before and after eating or drinking.
- We identified numerous barriers to adopting these protective behaviors, including inconsistent access to clean hand washing and bathroom stations with soap, water, and towels.
- Some participants reported bringing their own water and/or using hand sanitizer to wash their hands. The WPS states that hand sanitizer may not remove pesticide residues on hands.
- Current WPS regulations are not clear and require “ample” access to water, soap, and towels, without information about what “ample” means.
- There are no specific sanitation requirements for bathrooms. Participants shared concerns regarding the cleanliness of the toilets. Some reported solutions such as going to the bathroom in the field.
- Current regulations regarding access to hand wash stations should be clarified, and additional regulations regarding access to bathrooms should be developed and enforced to ensure workers have consistent access hand wash stations and bathrooms that are clean and safe.
References
- Arcury, T.A., J.G. Grzywacz, H. Chen, et al., Variation across the agricultural season in organophosphoruspesticide urinary metabolite levels for Latino farmworkers in eastern North Carolina: project design anddescriptive results. American journal of industrial medicine, 2009. 52(7): p. 539-550.
- Arcury, T.A., J.G. Grzywacz, S. Isom, et al., Seasonal variation in the measurement of urinary pesticidemetabolites among Latino farmworkers in eastern North Carolina. Int J Occup Environ Health, 2009. 15(4): p.339-50.
- Arcury, T.A., J.G. Grzywacz, J.W. Talton, et al., Repeated pesticide exposure among North Carolina migrant andseasonal farmworkers. American journal of industrial medicine, 2010. 53(8): p. 802-813.
- Arcury, T.A., P.J. Laurienti, H. Chen, et al., Organophosphate Pesticide Urinary Metabolites Among LatinoImmigrants: North Carolina Farmworkers and Non-farmworkers Compared. J Occup Environ Med, 2016. 58(11):p. 1079-1086.
- Arcury, T.A., H. Chen, P.J. Laurienti, et al., Farmworker and nonfarmworker Latino immigrant men in NorthCarolina have high levels of specific pesticide urinary metabolites. Arch Environ Occup Health, 2018. 73(4): p.219-227.
- Krenz, J.E., J.N. Hofmann, T.R. Smith, et al., Determinants of butyrylcholinesterase inhibition amongagricultural pesticide handlers in Washington State: an update. The Annals of occupational hygiene, 2015.59(1): p. 25-40.
- McCauley, L., J.D. Runkle, J. Samples, et al., Oregon indigenous farmworkers: results of promotor interventionon pesticide knowledge and organophosphate metabolite levels. J Occup Environ Med, 2013. 55(10): p. 1164-70.
- Coronado, G.D., B. Thompson, L. Strong, W.C. Griffith, and I. Islas, Agricultural task and exposure toorganophosphate pesticides among farmworkers. Environmental health perspectives, 2004. 112(2): p. 142-147.
- Barrón Cuenca, J., N. Tirado, M. Vikström, et al., Pesticide exposure among Bolivian farmers: associationsbetween worker protection and exposure biomarkers. Journal of exposure science and environmentalepidemiology, 2020. 30(4): p. 730-742.
- Zhang, X., W. Zhao, R. Jing, et al., Work-related pesticide poisoning among farmers in two villages of SouthernChina: a cross-sectional survey. BMC Public Health, 2011. 11(1): p. 429.
- Kasner, E.J., J.M. Keralis, L. Mehler, et al., Gender differences in acute pesticide-related illnesses and injuriesamong farmworkers in the United States, 1998-2007. Am J Ind Med, 2012. 55(7): p. 571-83.
- Calvert, G.M., J. Karnik, L. Mehler, et al., Acute pesticide poisoning among agricultural workers in the UnitedStates, 1998–2005. American Journal of Industrial Medicine, 2008. 51(12): p. 883-898.
- Thundiyil, J.G., J. Stober, N. Besbelli, and J. Pronczuk, Acute pesticide poisoning: a proposed classification tool.Bulletin of the World Health Organization, 2008. 86(3): p. 205-209.
- Weber, J. and A. Castro-Escobar, National Worker Protection Standard: A Manual for Trainers of Agricultural Workers and Pesticide Handlers. 2016, Pesticide Educational Resources Collaborative (PERC).
- U.S. Environmental Protection Agency, Pesticides; Agricultural Worker Protection Standard Revisions. A Rule by the Environmental Protection Agency. 2015.
- Pesticide Education Resource Collaborative (PERC). Worker Protection Standard (WPS) for Pesticide Handlers. EPA Approval Number: EPA Handler PST 00031. 2018 [cited 2023 May 25]; Available from:
https://www.youtube.com/watch?v=z2RGYppZw_E.