Last September, and in January of this year, we wrote about a suite of initiatives aimed at improving the quality and transparency of the NIH-supported research that most directly engages human participants – clinical trials. These initiatives include dedicated Funding Opportunity Announcements for clinical trials, Good Clinical Practice training, enhanced registration and results reporting on ClinicalTrials.gov, and required use of single IRB’s for multi-site studies. We are now entering the final phases of implementation of these initiatives – so, if you are contemplating research involving human subjects, please read on.
We’ve received queries from members of the research community seeking clarity on whether their human subjects research will be affected by these new policies, and if so, how. So, we want to call your attention to four questions researchers involved in human s studies need to ask, and answer. These questions are:
- Does the study involve human participants?
- Are the participants prospectively assigned to an intervention?
- Is the study designed to evaluate the effect of the intervention on the participants?
- Is the effect that will be evaluated a health-related biomedical or behavioral outcome?
If the answer to all four questions is yes, then we consider your research a clinical trial.
The NIH definition of a clinical trial is “a research study in which one or more human subjects are prospectively assigned to one or more interventions (which may include placebo or other control) to evaluate the effects of those interventions on health-related biomedical or behavioral outcomes”. The definition was published in 2014, after extensive public input, and affirmed, after even more public input, in our policypublished in September 2016. The clinical trial definition encompasses a wide variety of study types, as shown in figure 1. These range from mechanistic studies to behavioral studies, to pilot/feasibility studies, all the way to large-scale efficacy and effectiveness trials.
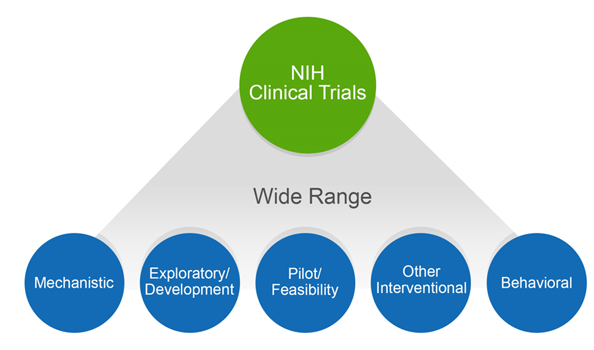
Figure 1
The breadth of the NIH definition is intentional, given the nature of the NIH portfolio and imperatives for maximal transparency. Transparency shows respect for the participants who put their trust in us, in the face of unknown outcomes, to help advance science. Our concerns about transparency stem in part from the issues surrounding the reporting of clinical trials data. For both NIH-funded and non-NIH funded trials, unreported data and untimely dissemination of results has been documented over and over again. Others have expressed concern that the NIH has not collected needed trans-NIH data to enable it to function as proper stewards of clinical trials.
Some have argued that we should not expect trial registration and reporting for small or exploratory trials, for trials that focus on safety, or for trials that fail to meet enrollment targets. As we stated last September, NIH chose to emphasize the value of transparency for these kinds of trials as well, as “the benefits of transparency and the need to fulfill the ethical obligation to participants is as relevant to these types of trials as to any other type.” We have an ethical obligation to report results, and this is especially true when volunteers contribute their time as study participants in prospective experiments, whether large or small. And, to be effective stewards of precious and constrained taxpayer monies, we need to collect a minimum of standardized data.
This transparency complements existing efforts to promote data sharing, public access to NIH-funded research results, and scientifically rigorous research design, all of which ultimately benefit the research community directly, as well. By developing and sharing robust data, we maximize the value of NIH’s investment in research by allowing scientists to build upon solid results. The definition, and our clinical trial policies, are an integral part of our efforts to enhance scientific stewardship, dissemination of information, transparency, and to excel as a federal science agency that manages for results.
Why is it important to know whether you are proposing to conduct a clinical trial? Correctly identifying whether your study is a clinical trial is crucial to complying with NIH policies, many of which are now in effect, such as registering and reporting all NIH supported clinical trials in ClinicalTrials.gov and good clinical practice training. Very soon, your answer will be crucial to picking the appropriate NIH funding opportunity for your application, writing your research plan correctly (since some information will be captured in the new human subjects and clinical trials form), and ensuring that your application includes all the information required for peer review.
If you are having difficulty answering the four questions that determine whether a study meets the NIH definition of a clinical trial, we encourage you to consult the case studies and FAQs that are available on our webpage on clinical trial requirements for grants and contracts. We’ll be following up with additional blogs and NIH Extramural Nexus articles that provide more depth on the various initiatives. We strongly encourage you to look at these materials, and share them with your colleagues, to ensure that as an awardee conducting clinical trial research, you are aware of the need to register your trial and report its results.