Ryan Williams, Madison Edwards, Dana Small, Shadee K. R. Edralin, Ian Tornello, Dr. Julia Oxford
Abstract:
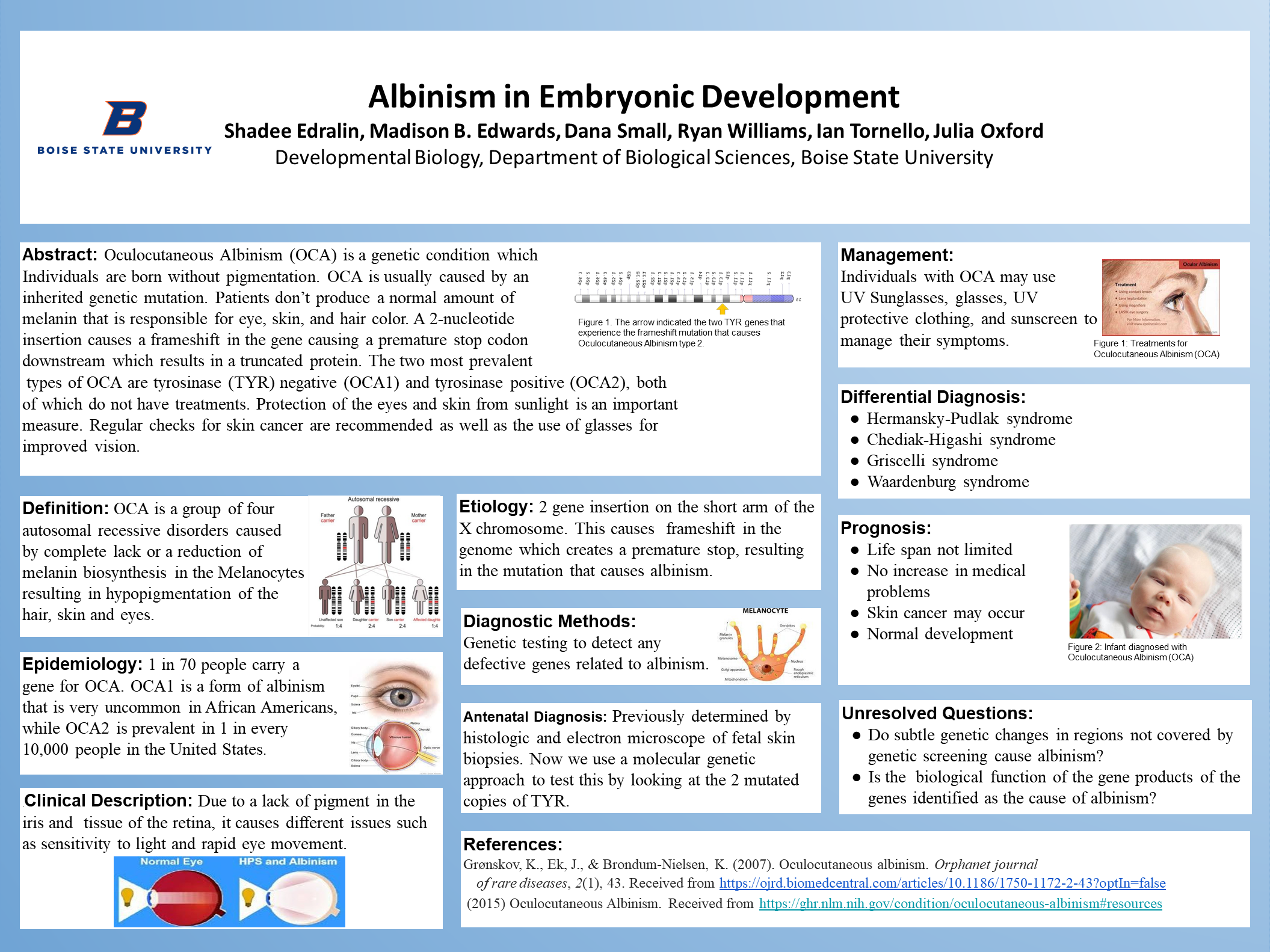
Oculocutaneous Albinism (OCA) is a genetic condition which Individuals are born without pigmentation. OCA is usually caused by an inherited genetic mutation. Patients don’t produce a normal amount of melanin that is responsible for eye, skin, and hair color. A 2-nucleotide insertion causes a frameshift in the gene causing a premature stop codon downstream which results in a truncated protein. The two most prevalent types of OCA are tyrosinase (TYR) negative (OCA1) and tyrosinase positive (OCA2), both of which do not have treatments. Protection of the eyes and skin from sunlight is an important measure. Regular checks for skin cancer are recommended as well as the use of glasses for improved vision.
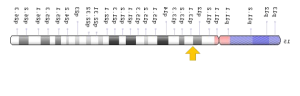
Definition:
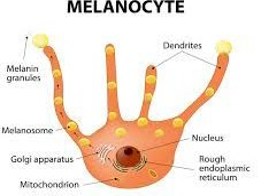
OCA is a group of four autosomal recessive disorders caused by complete lack or a reduction of melanin biosynthesis in the Melanocytes resulting in hypopigmentation of the hair, skin and eyes.
Epidemiology:
1 in 70 people carry a gene for OCA. OCA1 is a form of albinism that is very uncommon in African Americans, while OCA2 is prevalent in 1 in every 10,000 people in the United States.
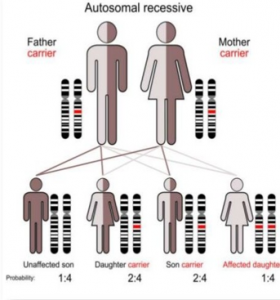
Clinical Description:

Due to a lack of pigment in the, iris and tissue of the retina, it causes different issues such as sensitivity to light and rapid eye movement.
Etiology:
2 gene insertion on the short arm of the X chromosome. This causes frameshift in the genome which creates a premature stop, resulting in the mutation that causes albinism.
Diagnostic Methods:
Genetic testing to detect any defective genes related to albinism.
Antenatal Diagnosis:
Previously determined by histologic and electron microscope of fetal skin biopsies. Now we use a molecular genetic approach to test this by looking at the 2 mutated copies of TYR.
Management:
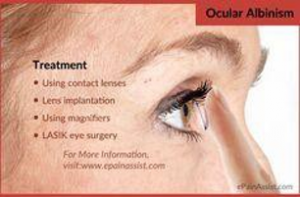
Individuals with OCA may use UV Sunglasses, glasses, UV protective clothing, and sunscreen to manage their symptoms.
Differential Diagnosis:
- Hermansky-Pudlak syndrome
- Chediak-Higashi syndrome
- Griscelli syndrome
- Waardenburg syndrome
Prognosis:

- Life span not limited
- No increase in medical problems
- Skin cancer may occur
- Normal development
Unresolved Questions:
- Do subtle genetic changes in regions not covered by genetic screening cause albinism?
- Is the biological function of the gene products of the genes identified as the cause of albinism?
References:
Grønskov, K., Ek, J., & Brondum-Nielsen, K. (2007). Oculocutaneous albinism. Orphanet journal of rare diseases, 2(1), 43. Received from https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-2-43?optIn=false (2015) Oculocutaneous Albinism. Received from https://ghr.nlm.nih.gov/condition/oculocutaneous-albinism#resource